Very good question. I was sent this article: The anabolic response to protein ingestion during recovery from exercise has no upper limit in magnitude and duration in vivo in humans, by Jorn Trommelen, et. al., which questions the validity of our current consensus as to the amount of protein that humans can absorb in one meal. This article landed in my inbox because I had said at a presentation that research shows that humans can only absorb ~30 grams of protein from a meal. The suggestion from the email was that I needed to keep up with the times and change my data.
I took an afternoon to read the article, review the multitude of charts, and read some of the citations. At first, it looks like very promising new data, however, there are a few questions I had about the methodology that may not have such positive outcomes.
What is a protein?
Just to be sure we are all on the same chemistry page, here is information about proteins. Proteins are not special. The term means that at least 100 amino acids got together to create a molecule. Digestion breaks down proteins into amino acids when the body needs this smaller unit.
Back to the research –
My 30-gram number is based on past research. That research also illustrates that if you eat more protein, the extra amino acids that are produced from digestion are oxidized. Oxidized molecules actually quiver and quake. This “quaking” can cause damage to cells, DNA, and, at the very least, increase your urine output creating stress in the kidneys and liver. Antioxidants such as Vitamin E, stop the quaking and decrease the stress oxidants put on the body.
What is new about this study?
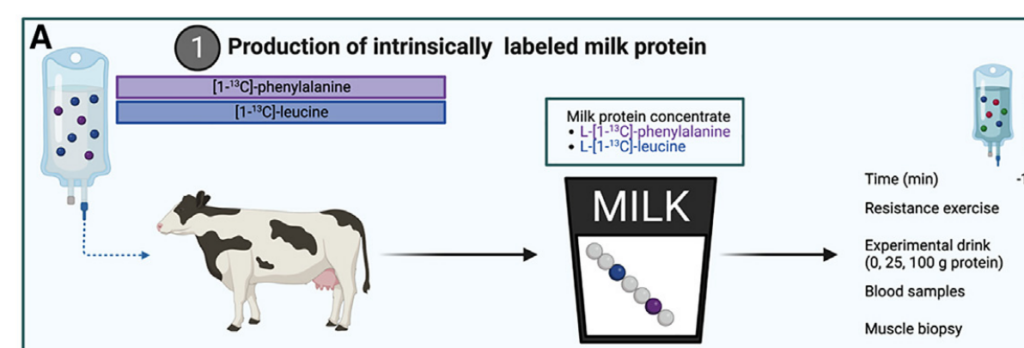
This new research used trace markers or dyes on the amino acids and followed them through the participants’ bodies. The additional protein ingested not only bypassed the oxidation problem but also made its way to muscle tissue. That is really interesting. Instead of increasing stress and urine output in the kidneys, the additional protein began to build muscle tissue.
According to the data, instead of 30 grams of protein, the body absorbed 100 grams of protein. Now, one caveat is that the body didn’t absorb it in a couple of hours, as seen in early research, but over 12 hours. In fact, the researchers stopped their tracing at 12 hours, so we don’t specifically know how long this continues nor how much protein was absorbed over time. It leads one to think that if you eat a boatload of protein at one time, you may not need to eat a concentrated protein food for a much longer time than we currently believe.
How does increased protein absorption affect bodybuilders?
I know some bodybuilders who eat every couple of hours. This data shows that the every 2-hour eating pattern may not be doing any additional good for the muscle tissue.
What patient needs the most amount of protein to recover?
As a dietitian, I was thinking about the use of these results in a clinical setting. Burn victims need the highest amount of protein. But, depending on the location and extent of their burns, eating and digestion may be extremely difficult. Could this data be implemented in this situation? That could be a game-changer. It may be useful for anyone having major surgery or needing to repair severe damage from an accident.
Here’s the other side of the coin.
First, and this is the least of the problems, the researchers begin their theory that the body can absorb more protein than previously thought by equating the digestive tract of humans to snakes. They theorize that since snakes eat their prey whole and take several days to digest all the proteins, why shouldn’t humans be able to absorb more protein over a longer period of time? They do state that there is a difference between reptiles and mammalian digestive tracts. Smart move.
Next, there were only 36 participants, and they were all healthy, non-smoking young men who exercised regularly. I’m not sure what that says about the rest of us. We know people over the age of 50 need more, a small amount more, of protein daily because they do not absorb it as well. What happens with that? Also, women’s bodies are different than men’s. What if you don’t exercise? Does it still work?
Where did the protein come from?
The participants were given a formulated high-protein food after a resistance exercise session. What did the researchers use as high-protein food? Altered Holstein milk. The researchers gathered bovine breast milk with the highest casein levels. Casein is one of the most abundant proteins in cow breast milk. It is absorbed slower than whey powder, and therefore, can build tissue over a longer duration.
That sounds great, doesn’t it? Well, except if you are part of the 70% of humans who are lactose intolerant. But the problems don’t stop there. Let’s take a closer look at casein, the hormone insulin-like growth factor – 1 [IGF-1], cancer, and bovine breast milk.
What is the connection between casein and cancer?[i]
Casein is approximately 80% of the protein in cow milk.[ii] Research has shown that when casein is added to the diet of mice with prostate and liver cancer, the growth of the cancer cells increases. In a petri dish of cancer cells, casein was the preferred food of the cells, causing them to proliferate until the casein was used up. Then the cancer cells stopped growing.[iii] These studies were done repeatedly using the average amount of casein found in cow milk. Our set of researchers didn’t use average casein levels in breast fluid. They deliberately gathered cow milk with the highest casein levels. What does the higher casein concentration do? Does it increase the proliferation of cancer?
In thinking back to the demographic that participated in this study, we see that Caucasians are much more tolerant of cow milk products. What about other populations?
There is a higher risk for Asians. There are clear risks of cancer among African Americans and milk consumption.[iv] However, race does not appear to be a major factor. Higher rates of cancer from those having the highest dairy ingestion are seen in the multiracial Adventists Health Study 2.[v] This is a massive study conducted by and for the Seventh-Day Adventist population in the United States. In this and other studies, the higher the cow milk consumption, the higher the risk of cancer, especially hormonal cancers.[vi]
How quickly do cancers occur?
Cancer does not happen in a week. Most people have cancer cells in their bodies sitting there dormant for decades. They need a catalyst to activate growth, grow enough to find a blood source to proliferate, and then metastasize throughout the body. Why would you ingest a food that is known to proliferate whatever cancer cells you have?
What is the connection between IGF-1 and cancer?
One of the most abundant hormones in dairy milk is Insulin-like Growth Factor-1 [IGF-1]. Humans have it, too. You have a lot when you are born. IGF-1 promotes growth. That’s a good thing precisely when you are born. The most amount of growth you will ever do in your life happens between your birthday and turning one year old. You will double in size. The IGF-1 aids in that growth.
Bovine breast milk is meant to turn a 60-pound calf into a 600-pound cow in 6 months. You are not a calf and do not need to grow that much in a year or at any other point of your life.
The amount of IGF-1 in the body decreases when you reach puberty.[vii] It makes sense. You aren’t growing anymore, so why have a substance that is supposed to “grow” cells?
When you ingest foods with IGF-1, what does your body do with the extra? It grows things like cancer cells and tumors. Cancer cells work like a copy machine that won’t turn off. Not only won’t it turn off, but the copies also become distorted and don’t resemble the original. IGF-1 has been found to proliferate many cancers including skin, thyroid, prostate, and breast cancer.[viii] [ix]
When looking at the outcomes of the study, the continued protein absorption is intriguing. As stated earlier, burn patients need the most amount of protein since they are rebuilding tissue, and depending on their injuries, the abundant need for protein is significant. Additionally, if they have burns that impede food intake and digestion, being able to have a liquid source that can be administered through a tube may be very helpful. On the other hand, if a person’s health is so compromised, would adding a known carcinogen to their foods be the best choice?
What would be truly of interest is if a non-casein and IGF-1 source, such as pea protein or soy milk, would have the same continuous absorption rate of protein and the creation of muscle tissue.
This is a good bit of research that starts the ball rolling, but I would not base my massive muscle development on a food that in time could have me fighting for my life.
[i] Park, S. W., Kim, J. Y., Kim, Y. S., Lee, S. J., Lee, S. D., & Chung, M. K. (2014). A milk protein, casein, as a proliferation promoting factor in prostate cancer cells. The World Journal of Men’s Health, 32(2), 76. https://doi.org/10.5534/wjmh.2014.32.2.76
[ii] Davoodi, S. H., Shahbazi, R., Esmaeili, S., Sohrabvandi, S., Mortazavian, A., Jazayeri, S., & Taslimi, A. (2016). Health-Related aspects of milk proteins. PubMed, 15(3), 573–591. https://pubmed.ncbi.nlm.nih.gov/27980594
[iii] Dairy products linked to increased risk of cancer | University of. (2022, May 6). https://www.ox.ac.uk/news/2022-05-06-dairy-products-linked-increased-risk-cancer
[iv] Fraser, G. E., Jaceldo‐Siegl, K., Orlich, M. J., Mashchak, A., Sirirat, R., & Knutsen, S. F. (2020b). Dairy, soy, and risk of breast cancer: those confounded milks. International Journal of Epidemiology, 49(5), 1526–1537. https://doi.org/10.1093/ije/dyaa007
[v] Fraser, G., Miles, F., Orlich, M., Jaceldo-Siegl, K., & Mashchak, A. (2019). Dairy Milk Is Associated with Increased Risk of Breast Cancer in the Adventist Health Study-2 (AHS-2) Cohort (P05-026-19). Current Developments in Nutrition, 3(Suppl 1), nzz030.P05-026-19. https://doi.org/10.1093/cdn/nzz030.P05-026-19
[vi] Fraser, G. E., Jaceldo‐Siegl, K., Orlich, M. J., Mashchak, A., Sirirat, R., & Knutsen, S. F. (2020b). Dairy, soy, and risk of breast cancer: those confounded milks. International Journal of Epidemiology, 49(5), 1526–1537. https://doi.org/10.1093/ije/dyaa007
[vii] Janssen, J. a. M. J. L. (2019). IGF-I and the endocrinology of aging. Current Opinion in Endocrine and Metabolic Research, 5, 1–6. https://doi.org/10.1016/j.coemr.2018.11.001
[viii] Christopoulos, P. F., Msaouel, P., & Koutsilieris, M. (2015). The role of the insulin-like growth factor-1 system in breast cancer. Molecular cancer, 14, 43. https://doi.org/10.1186/s12943-015-0291-7
[ix] Study of almost 400,000 confirms that higher blood levels of IGF-1 are a risk factor for several types of cancer. (2020, September 15). Haiku. https://www.ceu.ox.ac.uk/news/study-of-almost-400-000-confirms-that-higher-blood-levels-of-igf-1-are-a-risk-factor-for-several-types-of-cancer